658
Views & Citations10
Likes & Shares
A case
control study was conducted on maternal determinants of preterm labor at
Department of Obstetrics and Gynecology, in Sree Avitom Thirunal (SAT)
Hospital, Medical College, Thiruvananthapuram among 460 women (230 cases and
230 controls). All cases delivered between gestational age of 24-37 weeks were
taken as cases and next term delivery (gestational age beyond 37 weeks but
below 42 completed weeks) happened in labor room as controls from November 1st,
2012 to November 30th, 2013. All consecutive cases as per the case
definition and satisfying the inclusion exclusion-criteria are included in the
study till the sample size of 460 is attained. The association of family
history of preterm birth with preterm birth was found using univariate analysis
by chi square test and multivariable analysis by logistic regression method.
Primary objective of the study was to identify various risk factors for mothers
undergoing preterm delivery and the secondary objective was the role of family
history in the prediction of preterm labor. The family history of preterm birth
(OR-9.693 and 95% CI of 2.037-46.128, p value=0.004) and preterm labor has
significant association with the study. The role of maternal genetic study
in foetal health and pregnancy outcome is not clear. Williams et al. carried a study to investigate familial
recurrence of preterm labour, and analyse the relative contributions of
maternal and foetal genotypes and the risk of preterm delivery. From the study,
more
than 90% of cases and controls had no family history of preterm birth. When
comparing between cases and controls, the percentage of cases with a family
history of preterm birth was higher than that of control group. Preterm birth is a complex trait
with a significant familial component. So it is essential to anticipate preterm
labor and give appropriate counselling to the mother regarding the factors
which may contribute to preterm labor and regarding preventable etiological
factors and to conduct frequent antenatal checkups.
Keywords:
Preterm labor, Genetics, Family history, Preterm delivery
INTRODUCTION
Preterm
birth is also the most important of short and long term morbidities in
infants and children and can have long
term health consequences such as cerebral palsy, blindness, developmental
deficiencies including cognitive, learning and language deficits.
Prematurity
affects 1 in 10 births or 11% world wide and 40-75% of neonatal deaths. The
incidence of preterm delivery is rising worldwide because of increased
frequency of multiple births due to artificial methods of reproduction, more
working mothers, increased stress and medically induced prematurity. The
precise aetiologies of preterm labour remain elusive, limiting the development
of preventive and therapeutic strategies. Despite decades of research much of the
aetiology remains unknown and hence, the rate of premature births has not
decreased and existing data suggest that it is on the rise.
Family history of preterm labour
They concluded as the recurrence risk of
preterm birth was transmitted through the mother and a higher risk if the
mother was born preterm herself. There was no added risk with the father’s
previous history or genetic input. Other studies shows a significant increase
in risk children, whose siblings were affectedby preterm birth, because of
maternal and/or foetal genetic influences. This added risk still persists even
after adjustment for non-genetic environmental risk factors in families.
Study design
A case control design was followed for the
conduct of study in order to study the role of multiple risk factors on a
single outcome.
Study setting
The study was conducted at the Department of
Obstetrics and Gynaecology, Sree Avittom Thirunal (SAT) Hospital, Medical
College Thiruvananthapuram, a tertiary care referral teaching hospital in
Kerala.
Study population
Study population included 460 women admitted
in SAT Hospital, Thiruvananthapuram (230 women as cases and 230 women as
controls).
Period of study
The study period was from November 1st, 2012
to November 30th, 2013 at Sree Avittom Thirunal Hospital, Government Medical
College, Thiruvananthapuram.
Definition of case
Women in the age group of 18-35 who delivered
in SAT hospital at a gestational age of 24-37 weeks, gestational age estimated
by the patients’ last menstrual period (LMP). It was determined on the basis of
whether menstruation was regular or by ultrasonography detecting gestational
age of less than 12 weeks.
Definition of controls
Women whose delivery occurred in SAT hospital
at or beyond a gestation age of 37 but below 42 completed weeks, gestational
age estimated by the patients’ last menstrual period (LMP), additionally
confirmed by first and second trimester ultrasound.
Exclusion criteria
1. IUDs and still births.
2. Women not willing to
participate in the study.
Sample size
Based on a pilot study conducted at SAT
Hospital, Thiruvananthapuram.
n={Z1-α/2 √(2P ̅(1-P ̅ ) )+Z1-β √(P₁(1-P₁)+P₂(1-P₂)
)}2/(P₁-P₂)2
P1 = (OR×P₂)/(1+P₂(OR-1) )
P ̅=(P₁+P₂)/2
P2=
Proportion of exposure in control group
P1=
Proportion of exposure in cases
OR=
Odds ratio
α
= Significance level
1-β= Power
Taking a case control ratio of 1:1, 230 cases and 230 controls were
recruited for the present study (Table 1).
Selection
of cases and controls
All consecutive
cases as per the case definition and satisfying the inclusion - exclusion
criteria were included in the study till the sample size was attained. Women as
per the definition criteria for controls and those coming next to every case
was selected as controls.
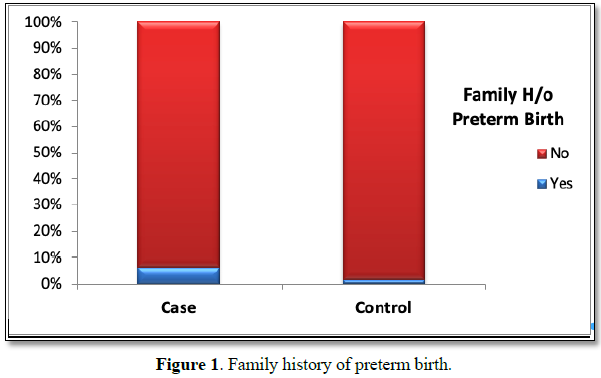
ASSOCIATION OF PRETERM BIRTH AND FAMILY HISTORY OF PRETERM LABOUR
Family history of
preterm birth
The study examined the association between family history of preterm
birth and present preterm birth. More than 90% of cases and controls had no family
history of preterm birth. When comparing between cases and controls, the
percentage of cases with a family history of preterm birth was higher than that
of control group and this difference in percentage was found to be
statistically significant by using the chi-square test. Odds ratio of 3.9 (p
value 0.010 and 95% CI=1.3-12.1) indicates that the chance of preterm birth was
nearly 4 times more among mothers who had a family history of preterm birth (Table 2 and Figure 1).
Data Analysis
The data was analysed using
descriptive and inferential statistics. The distribution of variables were
looked into and appropriate statistical significance test were undertaken. Collected
data was entered in MS EXCEL. Completeness was checked and analysis was done
using downloaded version of statistical software SPSS version 20. Qualitative
variables were expressed using proportions and quantitative variables in mean
and standard deviation. Quantitative
variables were categorized using suitable cut offs and analysed appropriately.
Test of association was done using
Chi square test and Fisher‘s exact test. Odds ratio and 95% confidence interval
was computed as the estimate of strength of risk. Logistic regression (Backward
stepwise method) was done as multivariable analysis to find out the significant
determinants after finding the collinearity of the variables.
RESULTS
A case control study
was undertaken to identify the various determinants of preterm delivery, during
the period 1st November 2012 to 30th November 2013 at SAT hospital,
Thiruvananthapuram. A total of 460 subjects were studied; 230 cases, women
delivered between 24-37 weeks of gestation and 230 controls, women who
delivered after 37 weeks but before 42 weeks. Distribution of study variables
in relation to case-control status were analysed. Chi-square test was used for
finding the association between the variables in the present study. Strength of
association of significant variables were presented using odds ratios with 95%
confidence interval after dichotomously categorizing them. This was followed by
the presentation of logistic regression analysis to find out the significant
determinants
DISCUSSION
The role of maternal
genetic study in foetal health and pregnancy outcome is not clear [1]. Carried
a study to investigate familial recurrence of preterm labor and analyse the
relative contributions of maternal and foetal genotypes and the risk of preterm
delivery. From the study, more than 90% of cases and controls had no family
history of preterm birth. When comparing between cases and controls, the
percentage of cases with a family history of preterm birth was higher than that
of control group and this difference in percentage was found to be
statistically significant by using the chi-square test. Odds ratio of 3.9
indicates that the chance of preterm birth was nearly 4 times more among
mothers who had a family history of preterm birth. In a study from 1974, the
sisters of women who delivered preterm appeared to be almost twice as likely as
sisters-in-law to themselves deliver prematurely [2]. Mother’s family history
could pose risk for preterm birth, according to a study by researchers from
Ben-Gurion university of the Negev and Soroka University Medical Centre. The
study published in American Journal of Perinatology followed 2300 mothers and
daughters over 22 years and found that the risk of preterm delivery was
significantly higher among 34 percent women whose mothers had a history of
preterm birth. In the present study, family history of preterm birth came out
to be a significant determinant with an adjusted Odds ratio of 9.693 with (95%
CI of 2.037- 46.128, p value=0.004). The strongest established risk factor for
PTD is a previous PTD (7), but women who themselves were born preterm or whose
sisters delivered prematurely have also been shown to be at increased risk of
delivering preterm (8-11). Despite recognition of a familial component to PTD,
the strongest established risk factor for PTD is a previous PTD (7), but women
who themselves were born preterm or whose sisters delivered prematurely have
also been shown to be at increased risk of delivering preterm (8-11). Despite
recognition of a familial component to PTD, the strongest established risk
factor for PTD is a previous PTD (7), but women who themselves were born
preterm or whose sisters delivered prematurely have also been shown to be at
in-creased risk of delivering preterm (8–11). Despite recognition of a familial
component to PTD, n the strongest risk factor for preterm labour is previous
preterm labour but the women who are themselves born preterm or whose sisters
delivered prematurely have also been shown to be at increased risk of
delivering preterm [3-6].
CONCLUSION
Preterm birth is a complex trait with a
significant familial component. So from the study it is established that if a
pregnant women has a family history of preterm labor, she is at significant
risk for preterm birth of her baby. So, it is essential to anticipate preterm
labor and give appropriate counselling to the mother regarding the factors
which may contribute to preterm labor and regarding preventable etiological
factors and to conduct frequent antenatal checkups. Thus, reducing the personal
expenditure and government expenditure in government hospitals by preventing
preterm births.
1. Williams MA, Mittendorf R, Lieberman E (1991) Monson
RR. Adverse infant outcomes associated with first-trimester vaginalbleeding.
Obstet Gynecol 78: 14-18.
2. Johnstone F, Inglis L (1974) Familial trends in low
birth weight. Br Med J 3: 659-661.
3. Porter TF, Fraser AM, Hunter CY, Ward RH, Varner MW
(1997) The risk of preterm birth across generations. Obstet Gynecol 90: 63-67.
4. Selling KE, Carstensen J, Finnström O, Sydsjö G (2006)
Intergenerational effects of preterm birth and reduced intrauterine growth: A
population-based study of Swedish mother-offspring pairs. BJOG 113: 430-440.
5. Winkvist A, Mogren I, Ho¨gberg U (1998) Familial
patterns in birthcharacteristics: Impact on individual and population risks.
Int J Epidemiol 27: 248-254.
6. Wilcox AJ, Skjaerven R, Lie RT (2008) Familial
patterns of preterm delivery: Maternal and fetal contributions. Am J Epidemiol
167: 474-479.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Proteomics and Bioinformatics (ISSN:2641-7561)
- Journal of Genomic Medicine and Pharmacogenomics (ISSN:2474-4670)
- Advances in Nanomedicine and Nanotechnology Research (ISSN: 2688-5476)
- Food and Nutrition-Current Research (ISSN:2638-1095)
- Journal of Agriculture and Forest Meteorology Research (ISSN:2642-0449)
- Journal of Astronomy and Space Research
- Journal of Biochemistry and Molecular Medicine (ISSN:2641-6948)